Pain and swelling from rheumatoid arthritis are reduced by 53% when patients adopt a vegan diet. The study's findings support that conclusion, as published in the American Journal of Lifestyle Medicine. Forty-four people with rheumatoid arthritis participated in the research.
They followed a vegan diet for four weeks. Finally, everyone avoided eating foods known to trigger inflammation for three weeks. During nine weeks, previously avoided foods were gradually reintroduced to one group.
The other group entered a supplementation stage. The reduction in edema and inflammation are seen among participants is interpreted as evidence that the dietary modifications were linked to clinical benefits, such as reduced swelling and better discomfort.
A Novel Research Examined Rheumatoid Arthritis Symptoms and Diet

Although prior research has shown a beneficial correlation between plant-based, anti-inflammatory diets and RA joint pain relief, this study is unique. It also included a crossover component in which the diet and placebo groups exchanged places after the initial trial run.
An Elimination Diet Removes and Reintroduces Suspicious Foods
Regarding vegetarian diets, the vegan one is the most stringent. Vegans don't just cut back on meat; they cut out entirely any food that comes from an animal. After four weeks of veganism, the elimination diet was the next drastic step for the diet groups.
Gluten, soy, white potatoes, sweet potatoes, chocolate, citrus, fruit, almonds, peanuts, onions, coffee, alcohol, and sugar were only some of the items that participants avoided.
To determine which foods were troublesome, participants reintroduced them one by one over nine weeks after a three-week vegan/elimination diet. Foods that were shown to be aggravating to the joints were taken out of the diet once again. They continued to eat it if it didn't make them sick.
Outcomes of Joint Pain Study Look Positive
Even after only four weeks on the vegan diet, both groups reported dramatic pain and joint swelling reductions. But, by pinpointing specific causes, they were able to further refine their meals with the use of the elimination diet.
In addition, the diet group dropped an average of 14 pounds, whereas the placebo group gained 2 pounds. Statistics showed a decrease in cholesterol with the vegan diet. Diet plays a crucial role in treatment. If you can regulate the patients' diet, inflammation will decrease.
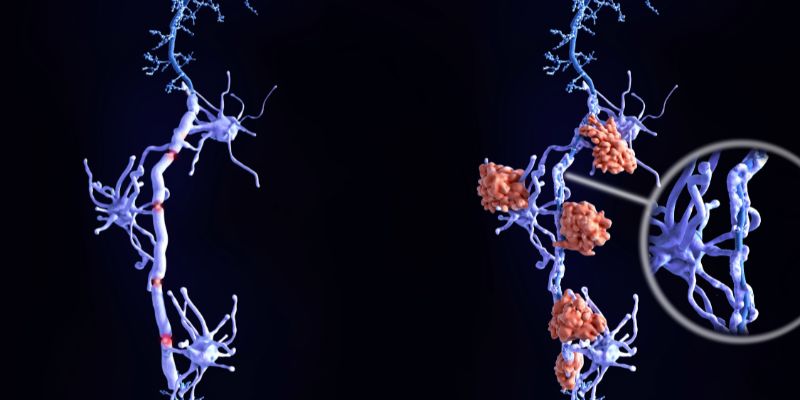
Plant-Based Diet Reduces Pro-Inflammatory Foods, Increases Anti-Inflammatory
There seem to be two mechanisms in the vegan diet contributing to symptom alleviation. The consumption of saturated fat is reduced on a plant-based, vegetarian, or vegan diet. You're not included butter, cheese, or milk fat in your diet, and you're not consuming any animal fats and substituting plant-based fats from sources like nuts and seeds for the saturated fats that can promote inflammation resulting in a diet that is more balanced and contains healthier fats.
Her second theory is that a plant-based diet reduces inflammation because its adherents consume more anti-inflammatory phytonutrients. All these minor plant molecules, like anthocyanin, have some influence on the body in terms of inflammation, not simply vitamin D and vitamin C.
Is More Research Needed?
This study has limitations that call for more investigation. Only 44 persons with RA were included in the research, and some didn't even fulfill the rules. While this is good research in terms of methodology, it is important to consider how generalizable the results are.
Instead of relying solely on clinical observation of disease activity, I believe biomarkers would be a more useful addition to the measuring toolkit. Landon, who has rheumatoid arthritis, warns that "clinical biomarkers" [such as blood levels of proteins that indicate systemic inflammation] would reinforce the investigations and results.
Maintaining A Vegan Diet Over Time Is Difficult.

Dr. Sandon also points out another issue: sticking to a vegan diet is difficult. A lot of folks give it a go and then give up. Without the right strategy, many people might have nutritional deficiencies. Patients with RA are already at increased risk for nutritional inadequacies. Therefore they shouldn't take any chances.
The protein intake must be sufficient. Insufficient vitamin and mineral intake is a problem. Dr. Bose says, "We urge our patients who desire to go vegan to do it step by step, especially if they were not previously vegetarian. Remove red meat from your diet first, and eventually, all other types of meat and fish.
Transitioning to a vegan diet can be challenging, so take your time. A diet you can stick to is better than one you can't, so vegetarianism is a good alternative if you can't keep it up. Consider other protein, calcium, B vitamins, and iron sources if you follow a vegan diet.